- History
- Physical Examination
- Diagnostic evaluation
- Differential Diagnoses of Abdominal Pain by Location
- Classification by acuity
History
- R/O catastrophic emergencies like AAA rupture
- Acute emergency vs acute non-emergent vs chronic
- Description
- Onset, progression, modulation
- Quality
- Location
- Associated symptoms
- ROS especially GI/GU
- PMH
- PSH
- Medications and allergies
- Comorbidities and Special populations – HIV, Pregnant, elderly, Sickle cell
Physical Examination
- Vitals
- Inspection
- Auscultation
- Palpation
- Percussion
- Rectal
- Pelvic
Diagnostic evaluation
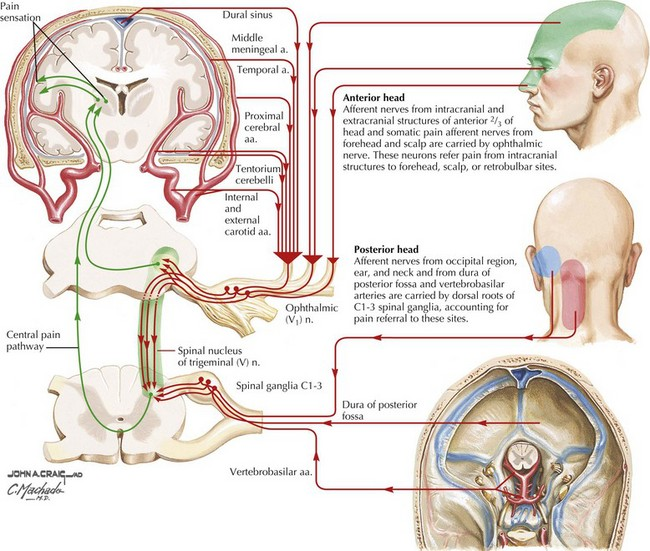
Anatomy

Differential Diagnoses of Abdominal Pain by Location
Right Upper Quadrant | Epigastric | Left Upper Quadrant |
Cholecystitis Cholangitis Pancreatitis Pneumonia/empyema Pleurisy/pleurodynia Subdiaphragmatic abscess Hepatitis Budd-Chiari syndrome | Peptic ulcer disease Gastritis GERD Pancreatitis Myocardial infarction Pericarditis Ruptured aortic aneurysm Esophagitis | Splenic infarct Splenic rupture Splenic abscess Gastritis Gastric ulcer Pancreatitis Subdiaphragmatic abscess |
Right Lower Quadrant | Periumbilical | Left Lower Quadrant |
Appendicitis Salpingitis Inguinal hernia Ectopic pregnancy Nephrolithiasis Inflammatory bowel disease Mesenteric lymphadenitis Typhlitis | Early appendicitis Gastroenteritis Bowel obstruction Ruptured aortic aneurysm | Diverticulitis Salpingitis Inguinal hernia Ectopic pregnancy Nephrolithiasis Irritable bowel syndrome Inflammatory bowel disease |
Diffuse Nonlocalized Pain | ||
Gastroenteritis Mesenteric ischemia Bowel obstruction Irritable bowel syndrome Peritonitis Diabetes | Malaria Familial Mediterranean fever Metabolic diseases Psychiatric disease |
|
Classification by acuity
Acute emergencies
Patients in whom there are concerns for life-threatening causes of abdominal pain should be referred to the emergency department.
These include those with:
- Unstable vital signs
- Signs of peritonitis on the abdominal exam (eg, abdominal rigidity, rebound tenderness, and/or pain that worsens when the examiner lightly bumps the stretcher)
- Concern that the abdominal pain is from a life-threatening condition (eg, acute bowel obstruction, acute mesenteric ischemia, perforation, acute myocardial infarction, ectopic pregnancy)
Evaluation of acute abdominal pain
- See DD according to location
- Diffuse?
- Further evaluation will depend on the results from the initial evaluation. As examples:
- Patients with a history concerning for IBD with extraintestinal manifestations and/or family history should be evaluated as appropriate. (See UptoDate)
- The combination of metabolic acidosis and elevated blood glucose strongly suggests diabetic ketoacidosis (DKA) as the etiology of the symptoms. It is important to keep in mind that an intraabdominal infection could precipitate DKA in a patient with diabetes. (See UptoDate)
- Patients with hyponatremia or hyperkalemia and symptoms of fatigue, malaise, nausea and vomiting, and symptoms of hypotension may have adrenal insufficiency. (See UptoDate)
- Hypercalcemia can cause abdominal pain, either directly or as an etiology for pancreatitis or constipation.
Evaluation of chronic abdominal pain
- Initial work up
- CBC
- CMP
- Amylase and lipase
- Iron Studies
- Anti-tissue transglutaminase
- Subsequent work-up
- < 50 IBS? Or more work up
- > 50 need further workup including imaging due to the age factor
- Less common causes of abdominal pain (table in Uptodate) should be considered in patients with repeated visits for the same complaint without a definite diagnosis, in an ill-appearing patient with minimal or nonspecific findings, in patients with pain out of proportion to clinical findings, and in immunocompromised patients. Examples of such cases include:
- Right upper quadrant pain after cholecystectomy mimics biliary colic and could be functional biliary pain; it could also arise from the intermittent passage of stones that have formed in the bile ducts, the passage of sludge, or the sphincter of Oddi dysfunction.
- Chronic, partial small bowel obstruction may occur in some patients. Patients usually present with chronic postprandial abdominal discomfort and variable nausea. Abdominal distention and tympany may be present, but usually without any fluid or electrolyte derangements. (See Uptodate)
- Very rare causes of intermittent acute severe abdominal pain should be considered in the setting of a positive family history (eg, familial Mediterranean fever, hereditary angioedema, acute intermittent porphyria [AIP]); in the case of AIP, the diagnosis may be considered even without a family history of the disease.
Specific comorbidities
- Pregnancy
- Elderly
- HIV
- SCD